Cultural Travel Packages
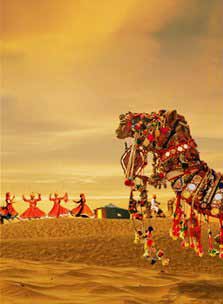
Numerous religions, ethos, customs, traditions, food, languages, castes etc have made India unique and diverse. The country is renowned worldwide for being culturally rich and vivid. From sparkling Golden triangle tour to eclectic North India trip – Our designed Indian cultural holiday packages intent to let the travelers seek genuine insights of various culture of the country.
-
1
Classical India Tour
10 Nights - 11 Days
1
Classical India Tour
10 Nights - 11 Days
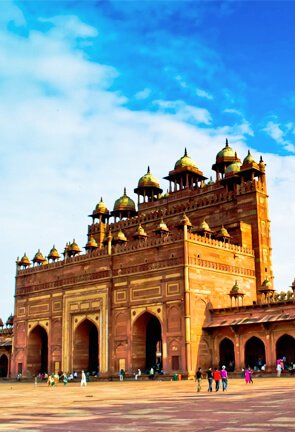
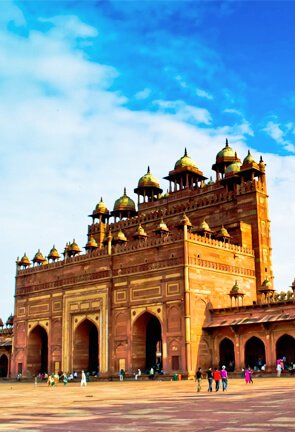
Discover India’s rich culture and heritage as Classical India Tour takes you to its best landmarks. The 10 days 9 nights package will tour you around the wonders of Indian cities like Delhi, Jaipur, Fatehpur Sikri, Agra, Jhansi, Orchha, Khajuraho and Varanasi. This tour will give you an insight to the religious and cultural heritage of incredible India.
view more
-
2
Golden Triangle Tour
05 Nights - 06 Days
2
Golden Triangle Tour
05 Nights - 06 Days
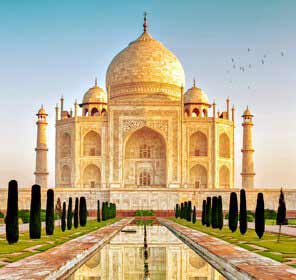
Explore the rich culture, tradition and history of India through the Golden Triangle Tour. This 5N/6D tour package will take you to tourist destinations like Delhi, Agra and Jaipur. Explore the historical forts, beautiful architecture and mesmerising mega structures. This tour will give you wonderful opportunity to sightsee some pride of India.
view more
-

3
Mystical India Tour
16 Nights - 17 Days
3
Mystical India Tour
16 Nights - 17 Days
Set sail to the mystical land of Indian tour. Explore the best of mystical India through our 16N/17D that will take you for an ultimate journey covering prominent states like Maharashtra, Gujarat, Rajasthan, Uttar Pradesh and Madhya Pradesh. Indulge in some interesting landmarks and visits forts, lakes, temples hill stations and lot more.
view more
-

4
Best of North India Tour
12 Nights - 13 Days
4
Best of North India Tour
12 Nights - 13 Days
Explore our thoughtfully designed 13 days 12 nights tour package that will give you a globetrot experience of India. Explore the historical sites in Delhi, witness the Flag Retreat Ceremony in Indo-Pak Wagah Border Amritsar; tour the forts in Jaipur, get inspired by the Taj in Agra, tour some fascinating temples of Khajuraho and cruise the Ganges to see the life of pilgrims.
view more
-
5
Best of Rajasthan
10 Nights - 11 Days
5
Best of Rajasthan
10 Nights - 11 Days
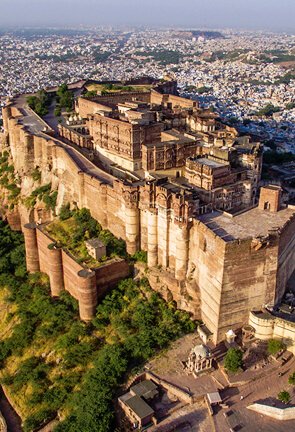
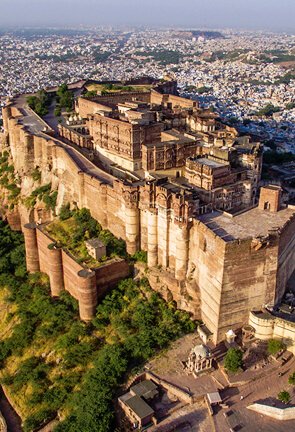
Rajasthan has the ability to charm and delight anybody who visits this enchanting place. We provide the best of Rajasthan tour in our 10N/11D expedition. Explore the magnificent rustic beauty of the desert, a boat ride at Lake Pichola in Udaipur; experience the forts of Jaisalmer and haveli’s in Bikaner, Nawalgarh and an elephant safari at Amber Fort in Jaipur.
view more
-

6
Travel with Ganges
8 Nights - 9 Days
6
Travel with Ganges
8 Nights - 9 Days
This tour package will provide you great spiritual experience to explore the various attractions of major riverfront cities in India like Delhi, Mathura, Agra, Varanasi, Allahabad and Lucknow. This tour lets you visit three sacred rivers in India – Yamuna, Ganga and Gomti. Seek peace and feel spiritually enlightened in the bays of these divine places.
view more
-

7
Flavours of India
05 Nights - 06 Days
7
Flavours of India
05 Nights - 06 Days
Explore the overall effect of Indian impressions and experience the essence of different flavours of India. Travel to the famous tourist centres with tangy flavour that will last throughout your stay. Enjoy our thoughtfully designed 12 days/13 night’s tour to Delhi’s quintessential ambience and well-known tourist centre like Varanasi, Jaipur, Udaipur, Khajuraho, Jhansi and Agra.
view more
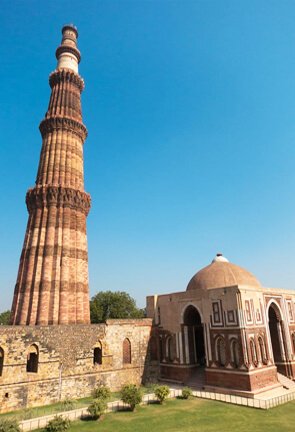
Heritage Travel Packages
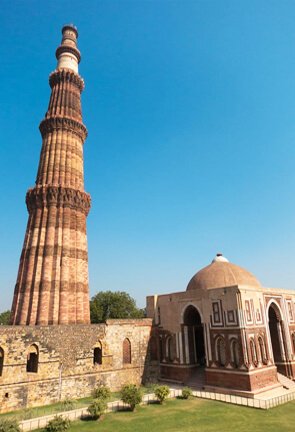
Capture the enigma of India by exploring treasures from the past built almost everywhere. India’s wide spectrum of heritage tourism acquaints tourists with the expansive vestiges – Forts, Palaces, Tombs and Temples of ancient empires calmly standing in the middle of vibrant cities of Central, Northern and Southern India. Our heritage holiday packages enable tourists to discover the ancient relics and architectural ruins of ancient India.
-

1
Forts and Palaces of Rajasthan
13 Nights - 14 Days
1
Forts and Palaces of Rajasthan
13 Nights - 14 Days
Visit abounding sites in Rajasthan with our 18D/17N tour package to some of the popular monuments nestled across Rajasthan such as the City Palace, Palace of Winds, Amer Fort, Nawalgarh Fort and various other famous attractions, enjoy a mesmerising event visiting Forts and Palaces of Rajasthan.
view more
-

2
Hidden Treasure Of Central India
12 Nights - 13 Days
2
Hidden Treasure Of Central India
12 Nights - 13 Days
Explore the hidden treasures of central India in our thoughtfully designed number of divine destinations to venture on your 13D/12N tour. During this expedition, you will be visiting some landmarks in popular destinations like Mumbai, Aurangabad, Ajanta, Indore, Ujjain, Sanchi, Bhopal, Jhansi and Gwalior.
view more
-

3
Southern Heritage Tour
11 Nights - 12 Days
3
Southern Heritage Tour
11 Nights - 12 Days
Travel to the south Indian states this vacation and join our tour for a heritage excursion. Explore the southern states in our 12D/11N and sightsee fabulous heritage sites in the cities like Bangalore, Srirangapatnam, Mysore, Chikmagalur, Hospet, Hampi, Hospet, Bijapur, Badami and Goa. Walk the ruins of age old history and important temples.
view more
-

4
Best of Gujarat Heritage Tour
09 Nights - 10 Days
4
Best of Gujarat Heritage Tour
09 Nights - 10 Days
India's westernmost state Gujarat has numerous sacred sites and our tour package can help you to soak in spirituality and sightsee some of. Explore the best of Gujarat’s finest historical places. Explore the best of Gujarat in our 10D/9N package and visit places like Ahmedabad, Jambughoda, Chhota Udaipur, Uthelia, Bhavnagar, Palitana, Gondal and Wankaner.
view more
-

5
Heritage Tour of Orissa
05 Nights - 06 Days
5
Heritage Tour of Orissa
05 Nights - 06 Days
An East Indian state on the Bay of Bengal, Odisha is popularly known for its tribal cultures and ancient Hindu temples. You can traverse the heritage sites of Odisha with our 6D/5N excursion and witness the majestic Konark Temple, Chilka Lake, Pipili Village, Khandagiri and Udayagiri Cave etc.
view more
-

6
Places in Himalayas
8 Nights - 9 Days
6
Places in Himalayas
8 Nights - 9 Days
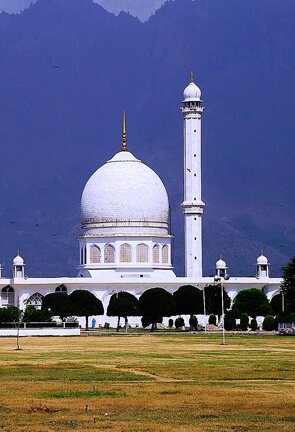
Explore many majestic palaces located in different parts of the Himalayan region with our 9D/8N Palaces of Himalayas Tour. Our package includes a visit to Taragarh Palace in Kangra Valley, the enchanting Dhauladhar Mountains, Bhagsunag Temple in Dharamshala followed by Dal Lake, Dalai Lama Temple and ancient Baijnath Temple in Pathankot.
view more
-

7
Highlights of Mumbai and Aurangabad
17 Nights - 18 Days
7
Highlights of Mumbai and Aurangabad
17 Nights - 18 Days
Explore the famous landmarks in these two Maharashtrian districts Mumbai and Aurangabad. Mumbai is adorned with magnificent monuments, beaches and Aurangabad stages Bibi Ka Maqbara and many other historical sites. Explore our 6D/5N tour package to spend a vacation witnessing and admiring the architectural beauties of Maharashtra.
view more
-

8
Historical Madhya Pradesh Tour
6 Nights - 7 Days
8
Historical Madhya Pradesh Tour
6 Nights - 7 Days
Madhya Pradesh, which preserves landmarks from eras throughout Indian history, is home to some incridable historical sites. With our tour package of 7D/6N journey to some notable landmarks and explore neighbourhoods like Bhopal, Bhojpur, Bhimbetka, Sanchi, Khajuraho, Orchha, Datia, Gwalior including other cities like Agra and Delhi.
view more
Kerala Holiday Packages
Unabashed climate flirting with the fertile soil letting everything blush in Kerala – God’s Own Country is an amazing place to witness some of the best wonders of nature. Our Kerala travel packages ensure that travelers get introduced with the Serene beaches, soul relaxing Ayurvedic treatments, beautiful tea gardens, majestic backwaters, exotic spices and rich culture.
-

1
Exotic Kerala Tour
09 Nights - 10 Days
1
Exotic Kerala Tour
09 Nights - 10 Days
This enchanting destination illustrates the beauty of nature, alluring beaches, beautiful palm trees and grand boathouses. Our 10D/9N Kerala tour will take you on a vacation to a world of rich greenery and tranquil backwaters. Explore the southern cities best landmarks from pristine backwaters to the hills and tea gardens.
view more
-

2
Kerala Honeymoon Tour
04 Nights - 05 Days
2
Kerala Honeymoon Tour
04 Nights - 05 Days
Explore your dream honeymoon vacation with your lover and explore the beautiful tropical paradise Kerala. Let our thoughtfully prepared itinerary for 5D/4N indulge you will a paradise like a holiday. Explore major romantic attractions of Kerala in some pristine destinations perfect for couples like Munnar, Thekkady, Alleppey Houseboat and Cochin.
view more
-

3
Magical Kerala Tour
06 Nights - 07 Days
3
Magical Kerala Tour
06 Nights - 07 Days
This wonderland surrounded by sandy beaches, peaceful backwaters and rich greenery is an unavoidable landing-place for nature lovers. Explore Kerala in our magical 6N/7D tour for quick introductory stops in divine places from hill station in Munnar, National Park in Periyar, backwater ride in Kumarakom and city tour in Cochin.
view more
-

4
Romantic Kerala Tour
06 Nights - 07 Days
4
Romantic Kerala Tour
06 Nights - 07 Days
With an undying natural beauty, calm backwaters, grassy forests and towering palm trees. Kerala, one of the most romantic getaways in the southern part of India hold mesmerising landscapes. Our 6N/7D tour will help you get to some major tourist destination in Kerala like Cochin, Munnar, Kumarakom, Kovalam and Trivandrum.
view more
-

5
Highlights of Kerala
03 Nights - 04 Days
5
Highlights of Kerala
03 Nights - 04 Days
Kerala is one of the most visited states in India and this tour of 3N/4D will guide you to its diverse attractive landmarks. Along the long stretch of the south Indian Territory experience, the leisure jaunt in its soothing ambience from the valleys of Munnar to the end of Kanyakumari.
view more
-

6
Wonders of Kerala
04 Nights - 05 Days
6
Wonders of Kerala
04 Nights - 05 Days
Explore the manifolds the state has to offer and 6N/7D is all it takes to delve into the fresh country and see its many destinations. From living in a boathouse in Alleppy to sunbathing on the sandy beach in Kovalam. Fill your soul with happiness around the best landmarks Kerala offers.
view more
-

7
Escape to Kerala
07 Nights - 08 Days
7
Escape to Kerala
07 Nights - 08 Days
Keep a steady pace when you are in Gods own Country and enjoy the 7N/8D escape to Kerala. In this tour, explore Kerala’s most unparalleled sight of the tea gardens in Munnar, the exotic wildlife of the Eravikulam National Park, the pristine beaches of Kovalam and scenic beauty of the backwaters.
view more
-

8
Enchanting Kerala
09 Nights - 10 Days
8
Enchanting Kerala
09 Nights - 10 Days
Experience beautiful Kerala in our 9N/10D excursion, our tour will showcase some enchanting treasures of the south. With immense vibrancy and tranquillity that is hard to miss explore pristine Munnar, traditional dance in Thekkady, beach in Kovalum, backwaters in Alleppey, sightseeing tour in Kanyakumari and city tour in Cochin.
view more
Honeymoon Tour Packages
Rich culture, wonderful landscape and amazing hospitality give many couples a reason to choose India to begin their marital bliss. We have incorporated some of the beautiful and romantic beaches and hill stations of India in our honeymoon travel packages to make ensure that newly-weds enjoy each other’s company in a tranquil environment.
-

1
Kashmir Honeymoon Tour
06 Nights - 07 Days
1
Kashmir Honeymoon Tour
06 Nights - 07 Days
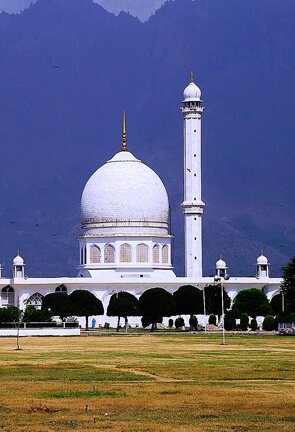
Paradise on earth Kashmir is a perfect place to for newlyweds to spend time together. Our 7 days 6 nights tour package includes a visit to idyllic lakes, snow coated mountains, picturesque gardens and calming ambience of abounding natural beauty. Explore some of the famous tourist spots of Kashmir and walk hand in hand through the captivating landmarks.
view more
-

2
Himachal Honeymoon Tour
07 Nights - 08 Days
2
Himachal Honeymoon Tour
07 Nights - 08 Days
Himachal Honeymoon tours which will give you access to spend an interesting honeymoon amidst peace and abundant scenic beauty. Our 7 nights 8 days package will let you tour around the beautiful hills of Shimla; witness rich flora and fauna of Manali; traverse the Pine and Deodar forest of Kullu and the gardens of Chandigarh.
view more
-

3
Uttarakhand Honeymoon Tour
06 Nights - 07 Days
3
Uttarakhand Honeymoon Tour
06 Nights - 07 Days
Surround yourself with snow covered mountains, high altitude lakes, rolling meadows, dense forests and rich flora and fauna in our Uttarakhand Honeymoon Tour package for a refreshing start with your spouse. Let our thoughtfully prepared itinerary for 6 nights 7 days honeymoon tour help you spend a dreamy vacation like never before.
view more
-

4
Kerala Honeymoon Tour
06 Nights - 07 Days
4
Kerala Honeymoon Tour
06 Nights - 07 Days
Delve into the sensual divine abode and enjoy our thoughtfully designed 9 days 10 nights honeymoon package to some of the exotic places in Kerala. Traverse the beautiful landmarks in places like Bombay, Cochin, Periyar, Kumarakom , Alleppey Marari and experience natural beauty of the south and memorial sites in Mumbai.
view more
-

5
Andaman Island Tour
06 Nights - 07 Days
5
Andaman Island Tour
06 Nights - 07 Days
Appreciate the crystal clear water, endless white sand beaches and romantic sunset in Andaman Island Tour. Engage in our 6 nights 7 days Honeymoon tour thoughtfully designed for honeymooners that will take you to some of the best islands of the Andaman and leave you with many unforgettable memories.
view more
-

6
Sikkim Darjeeling Honeymoon Tour
05 Nights - 06 Days
6
Sikkim Darjeeling Honeymoon Tour
05 Nights - 06 Days
Feel the breezy winds, soothing atmosphere and witness the captivating hill stations of the North East India. Be ready to explore our 5 nights 6 days honeymoon tour to the beautiful vacationing destinations of North East and explore the unmissable landmarks of Kalimpong, Gangtok and Darjeeling.
view more
-

7
Romance in Rajasthan
04 Nights - 05 Days
7
Romance in Rajasthan
04 Nights - 05 Days
Traverse a romantic destination in Rajasthan and tour around Mount Abu and Udaipur in our 4 nights 5 days Rajasthan Honeymoon Tour. The meticulously crafted tour package let you enjoy the beauty of landmarks like Nakki Lake and Dilwara Temple in Mount Abu and Sun Set Point in Udaipur followed by city excursion.
view more
-

8
Goa Honeymoon Tour
05 Nights - 06 Days
8
Goa Honeymoon Tour
05 Nights - 06 Days
Goa is a marvellous tourist destination famous for its romantic beaches and this picture-perfect place could be your honeymoon paradise. With our 5 nights and 6 days getaway, we offer an unlimited and uninterrupted time with activities of your own choice and overnight stays at luxurious hotels. At this surreal Indian destination make your honeymoon memorable.
view more
Trekking Tour Packages
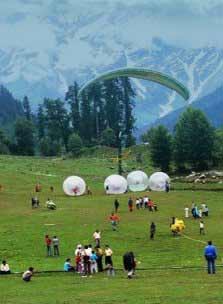
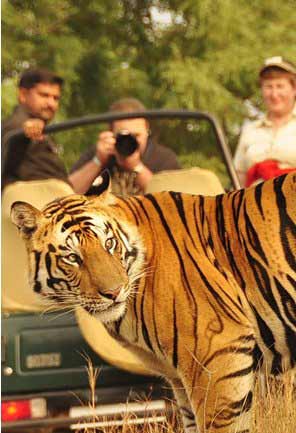
Explore the majestic paths of Garhwal and Kumaon; wander on the routes of Chamba and Manali; and get on the off beaten tracks of Ladakh and Zanskar in Jammu and Kashmir – the Himalayan foothills are ideal for trekking expeditions. Our trekking holidays ensure that adventurers discover the true nature of the country.
-

1
Trekking in Ladakh
50+ Treks
1
Trekking in Ladakh
50+ Treks
Spectacular razor sharp Mountains, dramatic curvy roads and bright blue sky - Ladakh is a paradise for adventurers and one can’t hide the head rush upon entering the Ladakhi trekking region. Undertake the regions flattery mountains trails and Frozen River amongst the countless rocky outcrops.
view more
-

2
Trekking in Garhwal
50+ Treks
2
Trekking in Garhwal
50+ Treks
Uttarakhand illustrates its spread out abundant natural beauty, viridian rivers, snow-capped peaks, waterfalls and rich meadow. Garhwal has a surplus of options for adventure holidays. Trekking in Garhwal Himalayas is one such activity that adds thrill in the destination.
view more
-

3
Trekking in Himachal
50+ Treks
3
Trekking in himachal
50+ Treks
Himachal is truly a perfect trekking adventure getaway. It's rich and high-spirited culture adds vastly to the beauty of the Himachal’s trekking Tour, besides it has plentiful adventure activities and trekking in Himachal is one of the oldest and the most favoured adventure tourism in the state.
view more
-

4
Trekking in Sikkim
20+ Treks
4
Trekking in Sikkim
20+ Treks
Pulsing with zestful of energy, Sikkim tourism has an undeniable extent when it comes to thrill and adventure tours. Drenched in the midst of diversity, travellers witness an unparalleled beauty and dramatic hills of the Himalayas. Sikkim offers an embrace with the cascading stream and rugged slopes experience most exhilarating trek of your lifetime.
view more
Religious Holiday Packages
Embarking on Chardham Yatra or a desire to retrace the path taken by Lord Buddha – India is the right country to begin a journey of enlightenment from various holy destinations. Discover the ‘Holy Bharat’ with our designed Pilgrimage holidays package to find the spiritual side of India.
-

1
Chardham Pilgrimage Tour
11 Nights - 12 Days
1
Chardham Pilgrimage Tour
11 Nights - 12 Days
Situated in the lap of Himalayas explore the four abodes in one of the most important pilgrimage route in the Indian Himalayas in Uttarakhand - Badrinath, Kedarnath, Gangotri and Yamunotri. Be a part of the Chardham pilgrimage tour and visit the important shrines and explore the radiant, magnetic view of the Himalayas.
view more
-

2
South India Temples Tour
11 Nights - 12 Days
2
South India Temples Tour
11 Nights - 12 Days
India’s great divine journey takes you to all the important temples in South India. South India Temple Tour gives an insight into the architectural excellence of southern temples that maintains an ambience to help you connect with the God. This tour will take you various temples like Lord Venkateswara, Govindaraja Swamy Temple, Arunachala Temple and much more.
view more
-

3
The Land of Lord Krishna
05 Nights - 06 Days
3
The Land of Lord Krishna
05 Nights - 06 Days
Mathura a sacred city in Uttar Pradesh is the deity Lord Krishna’s birth place. This tour will give you an insight of the holy journey; it will cover all the important godly places associated with Lord Krishna like Mathura, Nand, Gayon, Gokul, Barsana and Govardhan. The Land of Lord Krishna tour will bring peace and positivity to all visitors.
view more
-

4
Church Tour of South India
15 Nights - 16 Days
4
Church Tour of South India
15 Nights - 16 Days
India is a land of mixed culture and South India has a perfect blend of unity in diversity. This tour package will take you to some ornamented and wonderful architecture in various parts of the south region.
view more
-

5
Buddhist Pilgrimage Tour
09 Nights - 10 Days
5
Buddhist Pilgrimage Tour
09 Nights - 10 Days
Experience the distinctive atmosphere of the Buddhist Pilgrimage Tour. Stunning marvel structure elevates you as this tour takes you to catch a glimpse to some superb Buddhist pilgrimage sites. Experience tranquillity and peace as our tour package will take you to various Buddhist sites like Bodhgaya, Varanasi, Sravasti Kushinagar and Lucknow.
view more
-
6
Islamic Pilgrimage Tour
06 Nights - 07 Days
6
Islamic Pilgrimage Tour
06 Nights - 07 Days
Islamic Pilgrimage Tour will take you for rounds to catch a perfect glimpse of Islamic culture as you wander through the sites like Red Fort, Humayun’s tomb, Jama Masjid in Delhi. Explore the magnificent and remarkable Dargah Sharif in Ajmer and a pink city Jaipur where you stop at Amber fort.
view more
-

7
Jain Pilgrimage Tour
15 Nights - 16 Days
7
Jain Pilgrimage Tour
15 Nights - 16 Days
Jainism teaches to live life in harmlessness and renunciation and it is an ancient religion in India. Jain Pilgrimage Tour takes you to some of its opulent Jain Temples located in different areas. This perfect attempt to find serenity and spirituality are found in pristine areas like Bhavnagar, Junagarh, Mount Abu and Ajmer.
view more
-

8
Best of Sikhism Tour
13 Nights - 14 Days
8
Best of Sikhism Tour
13 Nights - 14 Days
India is a land where one can find a merger of different religions therefore the country is always lit with its vibrancy and culture. Best of Sikhism Tour will guide you to explore the shrines of Sikhism like Gurdwara Bangla Sahib and the Gurdwara Sis Ganj Sahib that illuminates a wonderful piece of architect and serenity.
view more
Beach Travel Packages
Sparkling clear water, swaying palm trees, and long coastline motivate tourists across the globe to spend pleasurable holidays on various beaches of Goa, Kerala and Andaman which range from gold to gravel. We offer amazing beach holiday packages to the tourists wishing to get acquaint with the shores of the country.
-

1
Port Blair, Havelock with Neil Island
05 Nights - 06 Days
1
Port Blair, Havelock with Neil Island
05 Nights - 06 Days
Go for an ultimate escapade from the city life and feel blessed with lush green forest and white sandy beaches of Andaman Island. This tour will provide you 5N 6D expedition to Port Blair, Havelock and Neil Island. Explore the city through our thoughtfully prepared itinerary help you spend a leisure and calm time with your family here.
view more
-

2
Golden Beaches of Goa
05 Nights - 06 Days
2
Golden Beaches of Goa
05 Nights - 06 Days
Enjoy the coastline of Goa's best beaches that attract visitors all year round. With our 5N and 6D tour at this prime location, sightsee Goa's perfect blend of Latin heritage, scenic beauty, amazing nightlife and engaging beaches. Tour around the northern and southern Goa and visit some of the landmarks widely popular in Goa.
view more
-

3
Best of India Beaches
10 Nights - 11 Days
3
Best of India Beaches
10 Nights - 11 Days
Overlooking the Arabian Sea or the Laccadive Sea, India is dotted with pristine beaches to help you lose your mind. This 10N and 11D tour provides you with best of Indian beaches. Take the trails to the best seashore of Mumbai, Goa, Kovalam, Varkala, Kochi and experience the beaches as well as historical sites in just one expedition.
view more
-

4
Golden Triangle with Goa
10 Nights - 11 Days
4
Golden Triangle with Goa
10 Nights - 11 Days
Experience the exotic beaches of Goa and historical sites in Delhi, Agra and Jaipur. This 10N and 11D Golden Triangle with Goa Tour will offer you a blend of rich cultural savoir-faire that transports you to a classical era. Explore some historical landmarks and dive in for a refreshing treat in some of Goa's best beaches.
view more


 10000+ tours
10000+ tours 24 hours services
24 hours services Customer experience:
Customer experience:







 250km
250km